Alzheimer’s disease – According to the Alzheimer’s Association, in the United States someone develops Alzheimer’s disease every 69 seconds, and by 2050 this is expected to increase to a new case every 33 seconds.Alzheimer’s disease is one form of dementia that gradually gets worse over time. It affects language, decision-making ability, judgment, memory, thinking and behavior.
Alzheimer’s disease – According to the Alzheimer’s Association, in the United States someone develops Alzheimer’s disease every 69 seconds, and by 2050 this is expected to increase to a new case every 33 seconds.Alzheimer’s disease is one form of dementia that gradually gets worse over time. It affects language, decision-making ability, judgment, memory, thinking and behavior.
There are two types of AD:
- In early-onset AD, symptoms first appear before age 60. Early-onset AD is much less common than late onset. However, it tends to progress rapidly. Early-onset disease can run in families. Several genes have been identified.
- Late-onset AD, the most common form of the disease, develops in people age 60 and older. Late-onset AD may run in some families, but the role of genes is less clear.
The first signs are forgetfulness, changes in language, memory and cognitive skills, change in social behavior, and difficulty with simple tasks. The cause of Alzheimer’s is not entirely known; however, research strongly suggests dietary and environmental causes, lack of exercise and a smaller percentage of cases being genetic. Other possible risk factors include: longstanding high blood pressure, physical inactivity, depression, low education, high blood pressure, diabetes, obesity, smoking history of head trauma, and being female.
Type 3 Diabetes
In an article titled Alzheimer’s; Diabetes of the Brain? Dr. DeLamonte investigated the links between insulin, genetics, nitrites and Alzheimer’s. We know that with diabetes, the cells become resistant to insulin causing the pancreas to increase the amount of insulin released. What people may not know, is that in Alzheimer’s, the part of the brain that is responsible for memory and personality also becomes resistant to insulin. Insulin is made in the brain in a similar way that it is made in the pancreas. In fact, insulin is responsible for helping build neurotransmitters and the tasks involved for learning and memory. Some researchers are now referring to Alzheimer’s disease as “type 3 diabetes.” Diabetics actually have up to a 65% higher risk of developing Alzheimer’s disease.
Genetics
According to Dr. DeLamonte, the majority of cases of Alzheimer’s disease is not genetic. When looking at the possible causes, it begins to make sense that Alzheimers can be prevented with proper diet and exercise. One of the major dietary causes connected to Alzheimer’s is the overexposure to nitrites in food, that convert to nitrosamines in the body; a known, deadly carcinogen. Nitrites are found in non-organic produce from chemical fertilizers, processed foods like hot dogs, deli meat, sausages, deli meats and non-organic beer. When performing experiments in the laboratory, Dr. DeLamonte found that very low, limited exposures to nitrosamines caused Alzheimer’s-type brain degeneration, dementia, diabetes, fatty liver disease and obesity.
Anticholinergic Drugs and Cognitive Decline
One study from the British Medical Journal looked at the use of anticholinergic drugs (nighttime pain relievers, antihistamines, sleep aids, antidepressants, incontinence drugs and narcotic pain relievers) and tested 372 people over 60 years old without dementia. A total of 9.2% of the subjects continually used anticholinergic drugs during the year before cognitive assessment. Compared with non-users, they had poorer performance on reaction time, attention, delayed non-verbal memory, narrative recall, visuospatial construction, and language tasks. Eighty percent of the continuous users were classified as having mild cognitive impairment.
Aluminum
Another major cause is the build up of aluminum, especially for those carrying the APO E4 gene allele (4 genes have been identified). Drinking water that is too acidic, high in monomeric aluminum and lacking in calcium, magnesium and silicic acid can create an environment that favors the uptake of aluminum. Avoiding aluminum cookware, canned and packaged foods, unfiltered water, deodorants that use aluminum are a few precautions to take to reduce aluminum exposure.
Coconut Oil
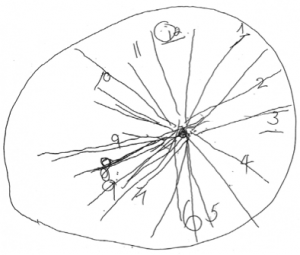
A case study done by Dr. Mary Newport titled What if there was a Cure for Alzheimer’s and No One Knew? focused on her husband’s advancing Alzheimer’s and the use of virgin coconut oil. In this study, she has him draw a clock on day 1, day 12, and day 37 while using coconut oil. From the pictures, you can see an incredible improvement.

Clock #2 14 Days after using virgin coconut oil
Clock #3 37 days after using virgin coconut oil
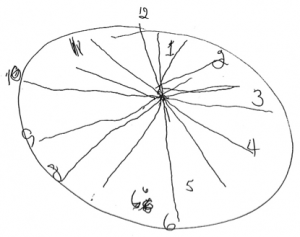
She also mentions that “instead of looking lost, he was involved and interested in what they had to say. He recognized relatives (brothers-in-law, nieces and nephews) by name immediately that were unfamiliar to him a year ago. His facial expression was more animated. He participated actively in conversations, understood jokes immediately and even came up with his own humorous comments. The dose was 35 grams or 2 tablespoons of coconut oil daily, and was used for cooking, added to oatmeal.
The best one I have found so far is Gold Label Virgin Coconut Oil from Tropical Traditions.
Further studies need to be done for testing ketone body b-hydroxy butyrate esters, since considerably higher levels of ketone bodies, timed and controlled could be achieved, and more ketones would be available for the neurons to use, and therefore greater improvement could be expected.
Avoid: All processed foods that contain sodium nitrites. This includes; hot dogs, lunch meat, sausages, bacon and most processed foods. Look for “nitrite free” when choosing any of these items.
Consume: Follow a diet rich in organic vegetables and fruit, wild salmon (order salmon with the highest purity in bulk here) free range chicken, grass-fed meat (bulk orders here), nuts, seeds and coconut oil with an emphasis on eating every 3-4 hours to keep blood sugar level. Minimize simple carbohydrate consumption (bread, crackers, cookies, muffins, tortillas, chips etc.) and grain consumption in general.
Exercise: Hiking, biking, swimming, weight training, gardening and any other physical activity is of paramount importance. Keep the body moving daily with any activity you enjoy for at least 45 minutes 4-6 times a week.
A very recent study called Reversal of Cognitive Decline: A Therapeutic Program has recently confirmed our approach with very significant results. This is the first time I have seen a study take grass-fed beef, wild fish and minimum grain consumption into consideration. Here is the synopsis and case studies:
Goal Approach Rationale and References
1. Optimize diet: minimize simple CHO, minimize inflammation. Patients given choice of several low glycemic, low inflammatory, low grain diets. Minimize inflammation, minimize insulin resistance.
2. Enhance autophagy, ketogenesis Fast 12 hr each night, including 3 hr prior to bedtime. Reduce insulin levels, reduce Aβ.
3. Reduce stress Personalized—yoga or meditation or music, etc. Reduction of cortisol, CRF, stress axis.
4. Optimize sleep 8 hr sleep per night; melatonin 0.5mg po qhs; Trp 500mg po 3x/wk if awakening. Exclude sleep apnea.
5. Exercise 30-60′ per day, 4-6 days/wk
6. Brain stimulation Posit or related
7. Homocysteine <7 Me-B12, MTHF, P5P; TMG if necessary
8. Serum B12 >500 Me-B12
9. CRP <1.0; A/G >1.5 Anti-inflammatory diet; curcumin; DHA/EPA; optimize hygiene Critical role of inflammation in AD
10. Fasting insulin <7; HgbA1c <5.5 Diet as above Type II diabetes-AD relationship
11. Hormone balance Optimize fT3, fT4, E2, T, progesterone, pregnenolone, cortisol
12. GI health Repair if needed; prebiotics and probiotics Avoid inflammation, autoimmunity
13. Reduction of Aβ Curcumin, Ashwagandha
14. Cognitive enhancement Bacopa monniera, MgT
15. 25OH-D3 = 50-100ng/ml Vitamins D3, K2
16. Increase NGF H. erinaceus (Lion’s Mane) or ALCAR
17. Provide synaptic structural components Citicoline, DHA
18. Optimize antioxidants Mixed tocopherols and tocotrienols, Se, blueberries, NAC, l-ascorbate (vitamin C), α-lipoic acid
19. Optimize Zn:Cu ratio Depends on values obtained
20. Ensure nocturnal oxygenation Exclude or treat sleep apnea
21. Optimize mitochondrial function CoQ or ubiquinol, α-lipoic acid, PQQ, NAC, ALCAR, Se, Zn, resveratrol, l-ascorbate, thiamine
22. Increase focus Pantothenic acid Acetylcholine synthesis requirement
23. Increase SirT1 function Resveratrol
24. Exclude heavy metal toxicity Evaluate Hg, Pb, Cd; chelate if indicated CNS effects of heavy metals
25. MCT effects Coconut oil or Axona CHO, carbohydrates; Hg, mercury; Pb, lead; Cd, cadmium; MCT, medium chain triglycerides; PQQ, polyquinoline
Patient #1
A 67-year-old woman presented with two years of progressive memory loss. She held a demanding job that involved preparing analytical reports and traveling widely, but found herself no longer able to analyze data or prepare the reports, and therefore was forced to consider quitting her job. She noted that when she would read, by the time she reached the bottom of a page she would have to start at the top once again, since she was unable to remember the material she had just read. She was no longer able to remember numbers, and had to write down even 4-digit numbers to remember them. She also began to have trouble navigating on the road: even on familiar roads, she would become lost trying to figure out where to enter or exit the road. She also noticed that she would mix up the names of her pets, and forget where the light switches were in her home of years.
Her mother had developed similar progressive cognitive decline beginning in her early 60s, had become severely demented, entered a nursing home, and died at approximately 80 years of age. When the patient consulted her physician about her problems, she was told that she had the same problem her mother had had, and that there was nothing he could do about it. He wrote “memory problems” in her chart, and therefore the patient was turned down in her application for long-term care.
(1) she eliminated all simple carbohydrates, leading to a weight loss of 20 pounds;
(2) she eliminated gluten and processed food from her diet, and increased vegetables, fruits, and non-farmed fish
(3) in order to reduce stress, she began yoga, and ultimately became a yoga instructor
(4) as a second measure to reduce the stress of her job, she began to meditate for 20 minutes twice per day
[5] she took melatonin 0.5mg po qhs
(6) she increased her sleep from 4-5 hours per night to 7-8 hours per night
(7) she took methylcobalamin 1mg each day
(8) she took vitamin D3 2000IU each day
(9) she took fish oil 2000mg each day
(10) she took CoQ10 200mg each day
(11) she optimized her oral hygiene using an electric flosser and electric toothbrush
(12) following discussion with her primary care provider, she reinstated HRT (hormone replacement therapy) that had been discontinued following the WHI report in 2002
(13) she fasted for a minimum of 12 hours between dinner and breakfast, and for a minimum of three hours between dinner and bedtime
(14) she exercised for a minimum of 30 minutes, 4-6 days per week.
Results
She began the protocol and was able to adhere to some but not all of the protocol components. Nonetheless, after three months she noted that all of her symptoms had abated: she was able to navigate without problems, remember telephone numbers without difficulty, prepare reports and do all of her work without difficulty, read and retain information, and, overall, she became asymptomatic. She noted that her memory was now better than it had been in many years. On one occasion, she developed an acute viral illness, discontinued the program, and noticed a decline, which reversed when she reinstated the program. Two and one-half years later, now age 70, she remains asymptomatic and continues to work full-time.
Patient #2
A 69-year-old entrepreneur and professional man presented with 11 years of slowly progressive memory loss, which had accelerated over the past one or two years. In 2002, at the age of 58, he had been unable to recall the combination of the lock on his locker, and he felt that this was out of the ordinary for him. In 2003, he had FDG-PET (fluoro-deoxyglucose positron emission tomography), which was read as showing a pattern typical for early Alzheimer’s disease, with reduced glucose utilization in the parietotemporal cortices bilaterally and left > right temporal lobes, but preserved utilization in the frontal lobes, occipital cortices, and basal ganglia. In 2003, 2007, and 2013, he had quantitative neuropsychological testing, which showed a reduction in CVLT (California Verbal Learning Test) from 84%ile to 1%ile, a Stroop color test at 16%ile, and auditory delayed memory at 13%ile. In 2013, he was found to be heterozygous for ApoE4 (3/4). He noted that he had progressive difficulty recognizing the faces at work (prosopagnosia), and had to have his assistants prompt him with the daily schedule. He also recalled an event during which he was several chapters into a book before he finally realized that it was a book he had read previously. In addition, he lost an ability he had had for most of his life: the ability to add columns of numbers rapidly in his head.
(1) he fasted for a minimum of three hours between dinner and bedtime, and for a minimum of 12 hours between dinner and breakfast
(2) he eliminated simple carbohydrates and processed foods from his diet
(3) he increased consumption of vegetables and fruits, and limited consumption of fish to non-farmed, and meat to occasional grass-fed beef or organic chicken
(4) he took probiotics
(5) he took coconut oil i tsp bid
(6) he exercised strenuously, swimming 3-4 times per week, cycling twice per week, and running once per week
(7) he took melatonin 0.5mg po qhs, and tried to sleep as close to 8 hours per night as his schedule would allow
(8) he took herbs Bacopa monniera 250mg, Ashwagandha 500mg, and turmeric 400mg each day
(9) he took methylcobalamin 1mg, methyltetrahydrofolate 0.8mg, and pyridoxine-5-phosphate 50mg each day
(10) he took citicoline 500mg po bid
(11) he took vitamin C 1g per day, vitamin D3 5000IU per day, vitamin E 400IU per day, CoQ10 200mg per day, Zn picolinate 50mg per day, and α-lipoic acid 100mg per day
(12) he took DHA (docosahexaenoic acid) 320mg and EPA (eicosapentaenoic acid) 180mg per day.
Results
He began on the therapeutic program, and after six months, his wife, co-workers, and he all noted improvement. He lost 10 pounds. He was able to recognize faces at work unlike before, was able to remember his daily schedule, and was able to function at work without difficulty. He was also noted to be quicker with his responses. His life-long ability to add columns of numbers rapidly in his head, which he had lost during his progressive cognitive decline, returned. His wife pointed out that, although he had clearly shown improvement, the more striking effect was that he had been accelerating in his decline over the prior year or two, and this had been completely halted.
Patient #3
A 55-year-old attorney suffered progressively severe memory loss for four years. She accidentally left the stove on when she left her home on multiple occasions, and then returned, horrified to see that she had left it on once again. She would forget meetings, and agree to multiple meetings at the same time. Because of an inability to remember anything after a delay, she would record conversations, and she carried an iPad on which she took copious notes (but then forgot the password to unlock her iPad). She had been trying to learn Spanish as part of her job, but was unable to remember virtually anything new. She was unable to perform her job, and she sat her children down to explain to them that they could no longer take advantage of her poor memory, that instead they must understand that her memory loss was a serious problem. Her children noted that she frequently became lost in mid-sentence, that she was slow with responses, and that she frequently asked if they had followed up on something she thought she had asked them to do, when in fact she had never asked them to do the tasks to which she referred.
(1) she fasted for a minimum of three hours between dinner and bedtime, and for a minimum of 12 hours between dinner and breakfast
(2) she eliminated simple carbohydrates and processed foods from her diet
(3) she increased consumption of vegetables and fruits, limited consumption of fish to non-farmed, and did not eat meat
(4) she exercised 4-5 times per week
(5) she took melatonin 0.5mg po qhs, and tried to sleep as close to 8 hours per night as her schedule would allow
(6) she tried to reduce stress in her life with meditation and relaxation; (7) she took methylcobalamin 1mg 4x/wk and pyridoxine-5-phosphate 20mg each day
(8) she took citicoline 200mg each day
(9) she took vitamin D3 2000IU per day and CoQ10 200mg per day
(10) she took DHA 700mg and EPA 500mg bid
(11) her primary care provider prescribed bioidentical estradiol with estriol (BIEST), and progesterone
(12) her primary care provider worked with her to reduce her bupropion from 150mg per day to 150mg 3x/wk.
Results
After five months on the therapeutic program, she noted that she no longer needed her iPad for notes, and no longer needed to record conversations. She was able to work once again, was able to learn Spanish, and began to learn a new legal specialty. Her children noted that she no longer became lost in mid-sentence, no longer thought she had asked them to do something that she had not asked, and answered their questions with normal rapidity and memory.
Recommended Supplementation for Alzheimer’s Disease
1. Memory Pro by Pure Encapsulations
Contains resveratrol, turmeric, ginkgo, lemon balm for rosemarinic acid, phosphatidly serine and Acetyl L-Carnitine.
Several epidemiological studies indicate that moderate consumption of wine is associated with a lower incidence of Alzheimer’s disease. Wine is enriched in antioxidant compounds with potential neuroprotective activities. The compound resveratrol is believed to be the therapeutic compound for Alzheimer’s.
In vivo data have clearly demonstrated the neuroprotective properties of the naturally- occurring polyphenol resveratrol in rodent models for stress and diseases. Furthermore, recent work in cell cultures and animal models has shed light on the molecular mechanisms potentially involved in the beneficial effects of resveratrol intake against the neurodegenerative process in Alzheimer’s disease.
In 2006, a study published in the Journal of Alzheimer’s Disease found that turmeric increased amyloid beta uptake of macrophages and might be a safe alternative to immune clearance of amyloidosis. Another study in 2009 found that vitamin D3 increased this ability further when combined with turmeric. There are actually 30 studies looking at the application of turmeric and Alzheimer’s.
In a double-blind placebo trial, 309 patients were included in the ITT analysis, 244 patients (76% for placebo and 73% for Ginko Biloba) for 26 weeks. In comparison to the baseline values, the placebo group showed a statistically significant worsening in all domains of assessment, while the group receiving 120 mg of Ginko Biloba was considered slightly improved on the cognitive assessment and the daily living and social behavior.
2. B-complex Plus by Pure Encapsulations
Scientists at the University of Oxford conducted a trial on 168 people and found that taking high doses of three vitamin B supplements every day reduced brain shrinkage associated with dementia by up to 53 per cent. Low folate and raised homocysteine concentrations in blood are associated with poor cognitive performance and result in neurotoxic and vasotoxic effects in dementia and Alzheimer’s disease suggesting that homocysteine is a direct marker for early cognitive decline. A randomized, double blind, placebo controlled study in the Netherlands looked at 818 subjects between 50-70 years old, and were given .8mg of folic acid for 3 years vs. a placebo. In the folic acid group, serum folate concentrations increased and plasma homocysteine decreased, while the improving the decline of cognitive function significantly.
3. Rosita Extra Virgin Cod Liver Oil or Fermented Cod Liver Oil if Carrying the ApoE4 Gene Variant
Researchers at Karolinska Institute and Uppsala University examined whether omega-3 supplementation had any effect on the psychiatric symptoms associated with Alzheimer’s disease. Specifically they looked at the agitation and depression often associated with Alzheimer’s disease. When they looked at all the patients with Alzheimer’s disease, they found no effect of omega-3 supplementation on symptoms of Alzheimer’s compared to the placebo group. However, when they separated the patients based on whether or not they carried the apoE4 variant, they found that carriers of the apoE4 gene variant responded positively to the omega-3 fatty acids with regard to agitation symptoms, while non-bearers of the gene variant showed an improvement in depressive symptoms.
A second study reported by French scientists in the November 13th 2007 issue of Neurology found that people who ate fish at least once a week had a 35 percent lower risk of Alzheimer’s disease and 40 percent lower risk of dementia, but only if they did not carry the ApoE4 gene variant. When choosing an omega-3 supplement, you want to make sure it is pharmaceutical grade and DOES NOT contain any heavy metals.
4. Vitamin C with Flavonoids by Thorne Research
Vitamin C converts nitrites into nitric oxide, preventing the formation of nitrosamines. Vitamin C is heavily concentrated in the brain, playing a major role in the production of GABA to reduce glutamate, that causes excitoxicity to the cells.
5. Lion’s Mane by Fungi Perfecti
Compounds in Lion’s Mane are able to stimulate the production of nerve growth factor (NGF), which promotes the repair and regeneration of neurons. There is growing clinical evidence that Lion’s Mane in beneficial in mild forms of dementia.
In a double blind placebo controlled trial, 50-80-year old Japanese men and women with mild cognitive impairment given 3g/day showed significant increases on a cognitive function scale compared with a placebo group over a 16 week period.
In another study, 7 patients with different types of dementia were given 5g a day of Lion’s Mane in soup. Six months all seven demonstrated improvement in their Functional Independence Measure score (eating, dressing, walking etc.), while six out of seven demonstrated improvements in their perceptual capacities (understanding, communication, memory, etc). You can supplement with Lion’s Mane, or purchase it in stores to add to meals.
Other Research
1. Astaxanthin by Pure Encapsulations:
A 2011 study in the British Journal of Nutrition showed that taking 6mg or 12mg of astaxanthin daily for 12 weeks lowered levels of phospholipid hydroperoxidases (compounds that accumulate in the red blood cells of people who suffer from dementia) by 40 percent and 50 percent respectively.
2. Ashwagandha by Pure Encapsulations:
Ashwagandha is a herb used in Ayurveda for a wide range of conditions. We use it in our practice mainly as an adaptogen for stress, however it has many more applications. Researchers at the National Brain Research Centre have indicated that Ashwagandha extract can reverse memory loss and become a promising cure for Alzheimer’s disease. In their study, they used two sets of mice (middle aged, and old) and were given Ashwagandha root extract for 30 days. After one month, there was a reduction of amyloid plaques (deposits found in the brain of individuals with Alzheimers) by improving a protein in the liver and cognitive abilities began to become restored. Initially the mice with Alzheimer’s were not able to learn or retain learning, and after 30 days they began to behave normally.
Patients with Alzheimer’s disease who receive high-dose vitamin E combined with a cholinesterase inhibitor have less long-term deterioration in their ability to perform activities of daily living than those who do not receive vitamin E, a new study found. Treatment benefit increased with time over five years, according to the authors of the study. This result may explain why some previous studies of vitamin E in patients with Alzheimer’s disease showed no effect after only one year, noted lead author Michael Flaherty in an interview with Medscape Internal Medicine. “Many neurologists continue to prescribe vitamin E for their Alzheimer’s patients, but whether it slows progression of dementia is unclear,” Mr. Flaherty said. “We found out there is promise for vitamin E in (fighting) this disease.” The studies that have shown the negative effects of vitamin E have all used synthetic vitamin E.
4. Vitamin K2 by Life Extension if Carrying the ApoE4 Gene Variant:
A particular gene variant called apoE4 is associated with increased risk of Alzheimer’s. However, this is just one of many gene variants that increase the risk of Alzheimer’s. While the apoE4 variant puts people at increased risk for Alzheimer’s disease, most people with Alzheimer’s disease have acquired it for reasons other than inheriting the apoE4 variant. Research how shown that people with he APOE4 gene may have a lower concentration of vitamin K which can inhibit nerve cell death due to oxidative stress. Although more research is needed, supplementation with vitamin K may prove beneficial to treating Alzeimer’s disease.5
5. Alpha-Lipoic Acid 600mg by Pure Encapsulations
A 2007 study published in the Journal of Neural Transmission found alpha lipoic acid “dramatically lowers” disease progression in Alzheimer’s disease patients who received 600mg a day for 12 months.
Sources
1. “Alzheimer’s Disease – PubMed Health.” 4 Oct. 2010. Web. 28 Apr. 2011. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001767/
2. http://www.doctoroz.com/videos/alzheimers-diabetes-brain?page=3#copy
3. Newport MD, Mary. “What If There Was a Cure for Alzheimer’s Disease and No One Knew?” 22 July 2008. Web. 28 Apr. 2011. http://www.coconutketones.com/whatifcure.pdf
4. “BioMed Central | Full Text | Therapeutic Potential of Resveratrol in Alzheimer’s Disease.” BioMed Central | The Open Access Publisher. Web. 28 Apr. 2011. <http://www.biomedcentral.com/1471-2202/9/S2/S6>.
5. Allison (2001). “The possible role of vitamin K deficiency in the pathogenesis of Alzheimer’s disease and in augmenting brain damage associated with cardiovascular disease.”. Medical hypotheses 57 (2): 151–5. doi:10.1054/mehy.2001.1307. PMID 11461163.
6. http://www.ayurvedictalk.com/ashwagandha-proven-to-be-a-potential-cure-for-alzheimers/2027/
7. Koseoglu E, Karaman Y. Relations between homocysteine, folate and vitamin B12 in vascular dementia and in Alzheimer disease. Clin Biochem. 2007; 40(12):859–863. [PubMed: 17532313]
8. Durga J, van Boxtel MP, Schouten EG, Kok FJ, Jolles J, Katan MB, et al. Effect of 3-year folic acid supplementation on cognitive function in older adults in the FACIT trial: a randomised, double blind, controlled trial. Lancet. 2007; 369:208–216. [PubMed: 17240287]
9. Ancelin, Marie L et al.Non-degenerative mild cognitive impairment in elderly people and use of anticholinergic drugs: longitudinal cohort study BMJ 2006; 332 doi: 10.1136/bmj.38740.439664.DE (Published 23 February 2006)